Value-based health care (VBHC) is a healthcare delivery model that prioritizes quality over quantity. Instead of paying providers based on the number of procedures performed, VBHC rewards them for achieving better patient outcomes.
The goal is simple: align the financial incentives of healthcare providers with patient needs. When implemented effectively, VBHC encourages preventive care, reduces complications, and shortens recovery times. By rewarding results rather than volume, it promotes efficiency and enhances the patient experience.
A Flexible Framework, Not One-Size-Fits-All
VBHC isn’t a rigid system. It’s a framework built on adaptable payment models suited to different healthcare contexts. Key payment approaches include:
- Value-Based Purchasing: Performance-based payment strategies that incentivize providers to meet benchmarks such as lower readmission rates and improved efficiency. Better performance equals financial rewards.
- Time-Driven Activity-Based Costing: Tracks costs at each stage of treatment, improving efficiency for procedures like carpal tunnel release. Benefits include better scheduling, shorter procedure times, reduced labor, and lower costs.
- Bundled Payments: Provide a fixed payment for an entire episode of care. For example, all treatments for a heart condition fall under one payment, encouraging holistic care and streamlined processes.
Together, these models align provider incentives with patient recovery, moving away from fee-for-service systems that often drive unnecessary treatments and higher costs.
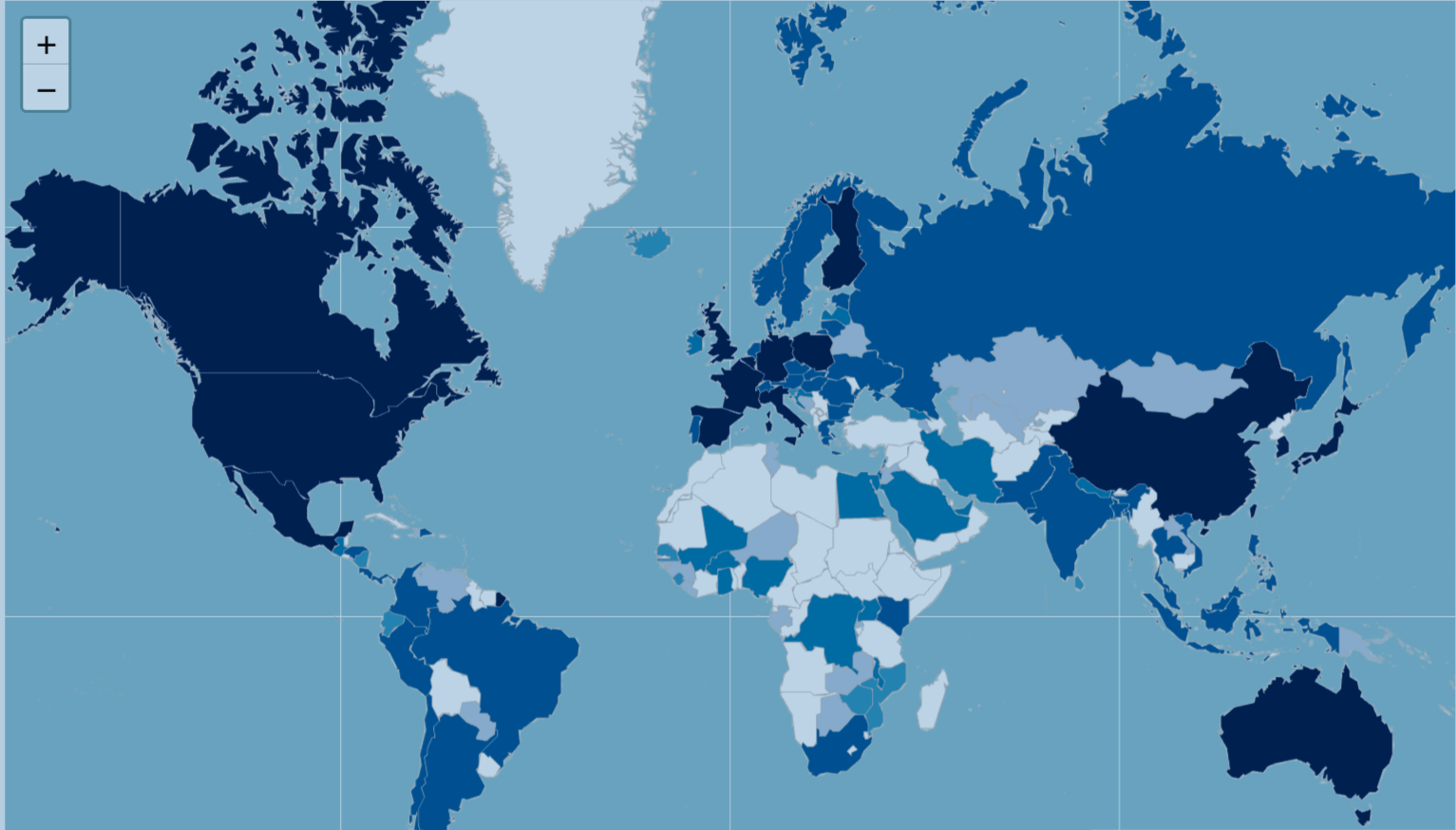
Global Progress and Adoption
Value-based health care remains in the early stages of adoption in many parts of the world. High-income countries, particularly the United States, have taken the lead, while progress in low- and middle-income regions has been slower due to infrastructure, financing, and policy constraints.
Implementation often begins locally within individual hospital departments or pilot programs, where change is more manageable. National-level initiatives, such as the Netherlands Heart Registry, remain relatively rare. Achieving broad, systemwide adoption will require significant structural reform and a cultural shift across healthcare systems.
Barriers and Enablers to Adoption
The transition to value-based care faces several challenges, including:
- Inadequate funding
- Weak financial incentives
- Resistance to change among healthcare professionals
- Outdated IT infrastructure
Many institutions still operate under legacy fee-for-service models that are deeply embedded and difficult to replace.
Despite these barriers, there are clear drivers supporting VBHC adoption. Studies show that VBHC can reduce costs and improve outcomes, particularly through shorter hospital stays and higher patient satisfaction. Patient-reported outcome measures provide valuable insights into care effectiveness from the patient’s perspective. At the same time, advances in digital health tools, data integration, and performance-based incentives are making it easier for providers to embrace the shift.
The Path Forward
VBHC is steadily gaining ground. While adoption remains uneven and gradual, most progress is concentrated in high-income settings and specific clinical areas. Operational and cultural barriers continue to slow broader implementation, but the potential is undeniable:
Better care. Lower costs. Greater accountability.
The growing use of patient-reported outcomes and digital infrastructure may accelerate adoption, but the current evidence base remains limited. Many studies are short-term, observational, and region-specific. To fully understand the impact and sustainability of VBHC, broader and longer-term research across diverse healthcare environments is essential. Only then can we unlock the full potential of value-based health care and transform healthcare systems worldwide.