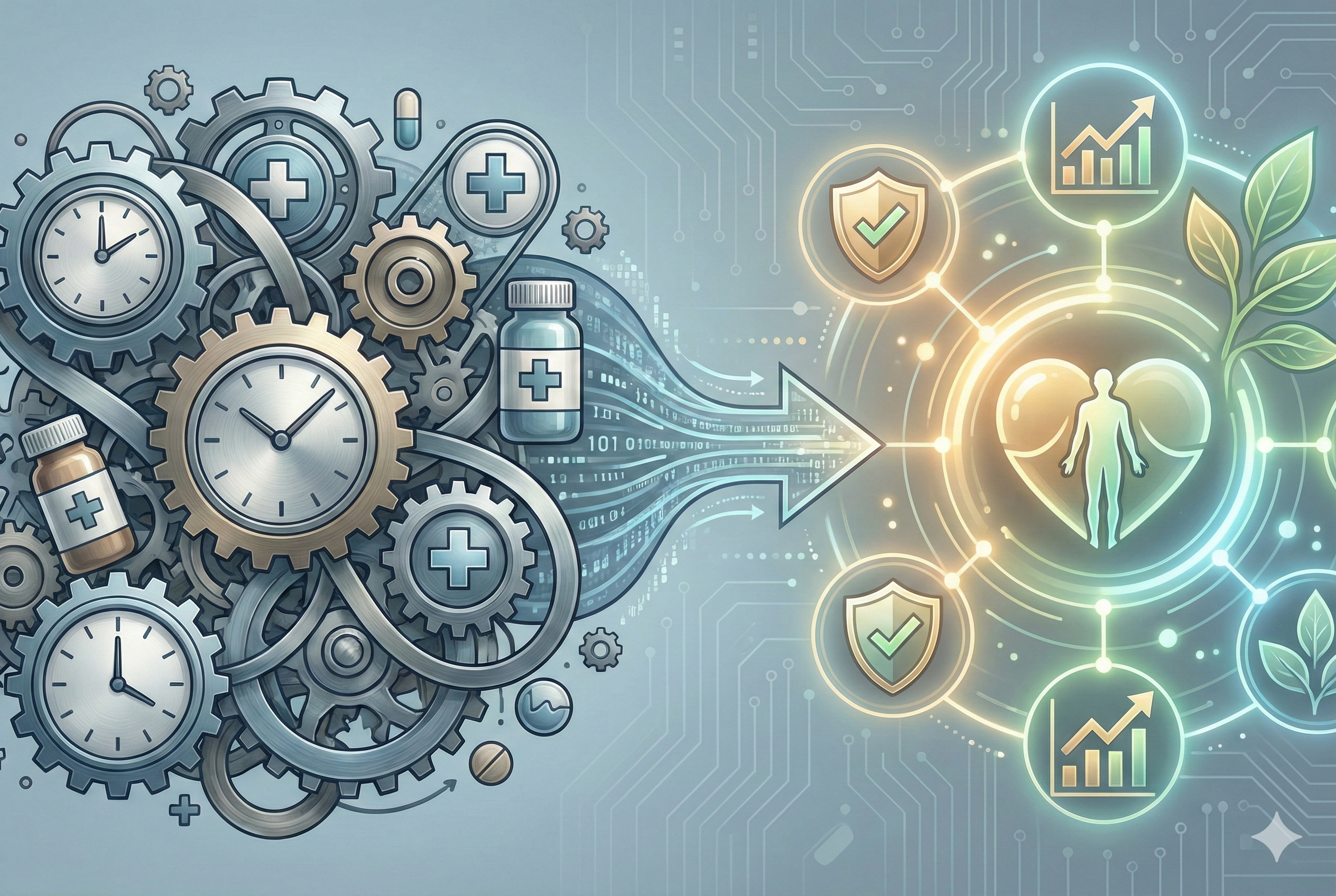
When a new treatment or technology comes to market, payers, Health Technology Assessment (HTA) agencies, and healthcare systems face a tough question: not just does it work? But can we afford it right now?
A budget impact model (BIM) helps answer the second question. These models estimate the short-term financial consequences of introducing an intervention, usually over a 1–5 year period. Unlike cost-effectiveness analyses, which focus on long-term value, BIMs are about near-term affordability.
What Budget Impact Models Measure
A BIM adds up the full cost of adopting a treatment. That includes:
- The manufacturing price of the drug or technology.
- Administration and monitoring.
- Managing potential side effects or complications.
- Offsetting savings, such as fewer hospitalizations or avoided disease-related costs.
The aim is simple: to show how a new option would change spending within a healthcare budget in the near term.
How They Differ from Cost-Effectiveness
Cost-effectiveness analysis looks at long-term outcomes using measures like quality-adjusted life years (QALYs) or incremental cost-effectiveness ratios (ICERs). A treatment can be highly cost-effective but still too expensive to adopt in the short run.
Budget impact models address this gap by focusing on the affordability question today, not ten years from now.
Key Elements of a Budget Impact Model
While the structure can vary, the best practice is to keep models as straightforward as possible while still credible. Common components include:
- Model structure – ranging from simple cost comparisons to more detailed decision trees or Markov models.
- Eligible patient population – defined clearly and projected over time, accounting for treatment success, dropout, or mortality.
- Treatment mix – how the new intervention fits with or replaces existing options.
- Costs – including acquisition, administration, monitoring, side effects, and disease-related costs.
- Sensitivity analyses – testing different assumptions to see how they affect results.
Why They Matter
For payers, HTA agencies and healthcare systems, BIMs are a reality check: can a new treatment be added without blowing up the budget?
For manufacturers, they are a way to demonstrate that a product isn’t just effective but also affordable enough to be reimbursed.
Because assumptions and inputs can differ, results may tell very different stories depending on who builds the model. That’s why transparency in data and methods is essential. Disagreements often lead to back-and-forth, with models refined until the assumptions are credible and acceptable to all sides.
The Bottom Line
Budget impact models provide a structured way to evaluate the short-term financial impact of new healthcare interventions. Used alongside cost-effectiveness analysis, they give decision-makers both perspectives they need: long-term value and immediate affordability.
In other words, BIMs are the financial reality check before saying yes to innovation.